Healing from trauma – a holistic approach based on Neuroscience
Are you seeking a path towards healing from trauma that is grounded in neuroscience and holistic understanding?
It’s not uncommon for clients to connect with me at a point where they have tried other forms of therapy and have left feeling unheard and unsupported. Sometimes this is because a therapist has provided ‘here and now’ solutions, but hasn’t addressed past emotions and experiences that are continuing to cause distress today.
The reality is that some experiences in our lives can leave lasting ripples that require a specialised approach – one that works with the interplay between our minds, emotions and bodies.
Often, when we’re healing from trauma, traditional talk therapies only touch the surface of how the brain and body hold and process this psychological pain. Without a holistic approach we can be left dealing with the overwhelming emotions, persistent somatic sensations, and the challenges of reconnecting with self, others, and the world around us.
If you’re on a journey of self-discovery and healing, please know that you’re not alone. In this blog post, we will explore the Neuroscience behind trauma healing and how a holistic approach based on Neuroscience can support healing from trauma.
What is trauma?
Most people have suffered or experienced a traumatic episode at some point in their lives (1). Derived from the Greek word meaning wound, the term trauma was previously used only for physical injuries. Now, it includes physical, emotional and psychological wounds.
A traumatic event or experience is one that poses a direct or perceived threat to life. Someone can experience trauma from a situation where they have felt threatened with serious injury, violence or even death.
Emotional and psychological trauma can occur from a range of experiences, including:
- threats to life or bodily integrity such as a violent encounter
- the death of someone close
- natural disasters
- accidents
- physical or sexual assault
- terrorism
- torture
- domestic violence
- childhood neglect
- hostage-taking
- sexual harassment of children, and
- diagnosis of a life-threatening illness.
Trauma can also occur from witnessing someone else’s safety being threatened.
The severity of trauma is influenced by many factors, including:
- a person’s perception of the event
- their age
- the type of abusive behaviour
- intensity, frequency, caregiving relationship, severity and duration of exposure to the traumatic event.
Further, factors include the person’s resources for bolstering resilience, and the emotional support available to them.
What is complex trauma?
Have you come across the term complex trauma? Let’s unpack what is meant by this.
Complex trauma emerges from ongoing interpersonal abuse, neglect or violence that occurs within caregiving or close relationships.
These trauma experiences can disrupt our attachment bonds and erode trust, impacting the development of our sense of self. This can lead to a loss of trust in self and in others, and because of this, complex trauma can contribute to the development of various mental health issues, such as:
- phobic disorders
- separation anxiety disorder
- oppositional defiant disorder, and
- attention deficit hyperactivity disorder in children
Complex trauma can also contribute to the development of post traumatic event disorders such as:
- depression
- bipolar
- antisocial or multiple personality disorders
- agoraphobia
- panic disorder and/or post-traumatic stress disorder (2)(3).
Researchers have also discovered that traumatic experiences within a family can affect future generations by changing our epigenetics. Epigenetics suggests that genes can be affected by changes to the epigenome and a set of biological factors. There is evidence to say that some traumas produce epigenetic changes that can be carried across generations making them predisposed to develop traumatic symptoms (4). For instance, researchers have shown that descendants of Holocaust survivors have been impacted through epigenetic inheritance of the trauma experienced by their ancestors (5).
This is why Psychotherapy now considers factors beyond the person’s individual experience of trauma, to look at traumatic events in someone’s social and family history as part of understanding and treating trauma.
How does trauma affect us?
Trauma breaks our sense of connection to ourselves (6), and can alter our perception of the world, and the people around us.
When someone experiences a traumatic event, their brain chemistry is altered, and the brain itself functions from its protective survival mechanisms.
While trauma responses are unique to each individual and each circumstance, there are some common signs of a trauma response.
If any of the below resonate with you, please remember that these responses are normal reactions to an abnormal and distressing event. If you are in distress, please connect with your healthcare professional (such as your doctor), mental health support lines and/or a therapist.
Emotional and psychological signs of trauma
- Shock, denial, or disbelief
- Confusion, difficulty concentrating
- Anger, irritability, mood swings
- Anxiety, fear and feeling on-edge
- Guilt, shame, self-blame.
- Withdrawing from others
- Feeling sad or hopeless
- Feeling disconnected or numb
Physical signs of trauma
- Insomnia and/or nightmares
- Fatigue
- Being startled easily
- Difficulty concentrating
- Racing heartbeat
- Edginess and agitation
- Aches and pains
- Muscle tension
As we can see, trauma doesn’t just impact our thoughts and emotions – it also has an impact on the body. This is why in trauma treatment, it’s so important to include the body in healing.
The Neuroscience of trauma
This next section is a bit Science-heavy, however I feel it’s important to share this information, so you can be informed about the ways in which trauma influences the brain.
Understanding the Neurobiology of trauma (how trauma affects the brain) helps to not only bust common misconceptions and to stop victim-blaming statements (that cause further pain), it can also explain many of the common behaviours and experiences of trauma survivors and helps us better understand the types of therapeutic treatments that can support trauma healing.
From a Neurobiological perspective, trauma is an overwhelming situation that creates an experience or pattern of experiences where the body’s automatic stress response systems are highly activated over such an extreme or prolonged time that they alter the regulation and functioning of the human Neurobiological system. (7)(8)
In 1994, Stephen Porges proposed the Polyvagal Theory, which shows us how trauma affects the body as well as the brain (6). This theory proposes that the vagus nerve (a core nerve within the Parasympathetic Nervous System) has two pathways, the Ventral and the Dorsal – each with different functions:
- the Ventral pathway responds to feelings of support, safety and social engagement, while
- the Dorsal vagal pathway responds to extreme danger.
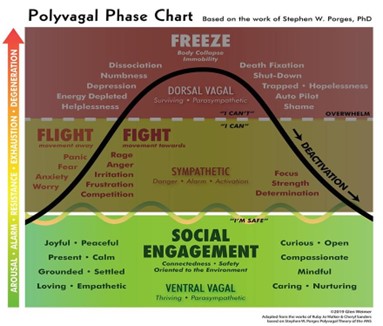
This can quite literally mean that the parts of our brain and body that are active when we’re in a restful state are ‘offline’ during a traumatic experience, while the body prioritises survival and finding the quickest perceived way to safety (fight, flight, or freeze).
It also provides compassionate insight into certain ways that we may respond to situations after a traumatic experience, for example, shutting down and being unable to move, or becoming defensive and angry.
That’s where trauma trained therapists can support individuals in an empathic and understanding way, to build awareness of these survival emotions, and through this, to start the process of healing.
Healing trauma – bridging Neuroscience and holistic healing
Trauma-informed therapies will often bring together Neuroscience with the body experience – recognising body wisdom as a crucial part of healing.
As the founder of Somatic Experiencing, Peter Levine says, “when therapeutic approaches focus mainly on thoughts, and neglect the body, the therapy will consequently be limited” (6).
In my practice as a trauma-informed Psychotherapist, I’ve witnessed the transformative impact of integrating Neuroscience and somatic awareness, with empathy and human connection – especially for clients who have not found traditional talk therapies helpful for processing their trauma.
Beginning with establishing safety, and always working at your pace, my therapeutic approach is based on a personalised and non-judgemental humanistic model, as well as contemporary Neuroscience. It is designed to guide you to a deepening connection with your emotions, behaviours and needs with the purpose of understanding where an emotion or behaviour is coming from. Whether the experience that led to it happened recently, or a long time ago, the ongoing emotion or behaviour is a sign that there is an unmet emotional or psychological need there.
By discovering the root, we can then compassionately acknowledge the stress or trauma that happened and learn how to meet those unmet needs – which starts the healing process.
Holistic therapy brings together mind, body, spirit and nature
Therapy sessions at Wise Beginning bring together the cognitive, emotional, somatic, relational, spiritual and nature aspects of the human experience.
Using a gentle method of inquiry, we can focus on sensations as the foundation of felt experience – supporting you to stay with your body processes and describe what you’re observing, while making meaning of your experience.
This can support you to identify and connect with your own needs and your internal dialogue, so that internalised messages, blocked memories and unresolved emotions from the past can be revealed.
The power of connection in healing
While trauma can isolate us, human connection has the power to heal. Creating a safe and compassionate space for healing is the cornerstone of my approach – where you can experience non-judgemental therapeutic connection as you process your pain.
Healing within the window of tolerance
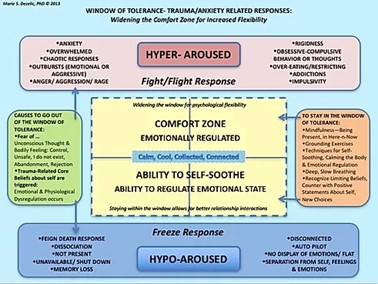
Neuroscience introduces the concept of the “window of tolerance,” as a space where healing can occur optimally. The window of tolerance describes space within which we are comfortable and feeling safe. It’s within this space, we are able to deal with the daily stressors of life, without feeling out of control.
It explains the normal brain/physiology reaction responses, as well in trauma-informed. Dezelic, M. (2013) Window of tolerance- Trauma/anxiety related responses: widening the comfort zone for increased flexibility. Retrieved from: https://www.drmariedezelic.com/window-of-tolerance--traumaanxiety-rela
To heal trauma, the nervous system should ideally be within this ‘comfort zone’, where we have access to our greatest amount of psychological flexibility and psychological safety.
By understanding each person’s window of tolerance during trauma therapy, I work with you to make sure that the healing process is both supportive and sustainable (that we’re not moving too far outside of this window and potentially causing more distress).
Self regulation and empowerment
Trauma can lead to disconnection from the body and the self. By drawing on Neuroscience-informed techniques, we can reset the nervous system and restore self-regulation. This can allow us to move from trauma survivors to empowered individuals who cultivate compassion for ourselves and embrace change.
Support to heal
If you’re seeking a way to heal from trauma that integrates Neuroscience, somatic awareness, and holistic understanding, I’m here to support you.
As an intuitive and open-minded Psychotherapist, I’m passionate about creating safe spaces and conversations where real and lasting healing can happen – where you can move at your own pace, in the direction of your best self, and your most connected and fulfilling relationships.
If you’re interested in Psychotherapy and Counselling, you can learn more about individual trauma counselling here, or get in touch with me here. I would love to support you to process your experience.
Alpha
Wise Beginning is a Psychotherapy and Counselling practice based in Brisbane in Australia.
Alpha offers sessions online and in-person, in both English and Spanish.
References and additional resources
24/7 SUPPORT:
Police, Fire or Ambulance – 000
Lifeline – 13 11 14
Kids Helpline – 1800 55 1800
Domestic Violence Hotline (QLD) 1800 811 811
- Levine, P. & Frederick, A. (1997). Walking the tiger: Healing trauma: The innate capacity to transform overwhelming experiences. California: North Atlantic Books.
- Fisher, J. (2017). Healing the fragmented selves of trauma survivors: Overcoming internal self – alienation. New York, NY: Routledge.
- Levers, L. L. (2012). Trauma Counselling: Theories and Interventions. Springer Publishing Company.
- Wolynn, M. (2016). It did not start with you: How inherited family trauma shapes who we are and how to end the cycle. New York, NY: Penguin Books.
- Jablonka, B. (2009). Transgenerational epigenetic inheritance: Prevalence, mechanisms, and implications for the study of heredity and evolution. The University of Chicago Press Journals 84(2) 131-176. Doi.org/10.1086/598822
- Levine, P. (2010). In an unspoken voice: how the body releases trauma and restores goodness.
- Chefetz, R. (2000). Affect Dysregulation as a way of life. Journal of the American Academy of Psychoanalysis, 28(2), 289-303. Doi/pdf/10.1521/jaap.1.2000.28.2.289
- Perry, B. D. (2008). Child maltreatment: A neurodevelopmental perspective on the role of trauma and neglect in psychopathology. In T. P. Beauchaine & S. P. Hinshaw (Eds.), Child and adolescent psychopathology (p. 93–128). John Wiley & Sons Inc.